Hiatal hernia is the protrusion or return of the upper portion of the stomach into the thoracic cavity, through the diaphragmatic (hiatal) orifice that communicates with the abdominal cavity.
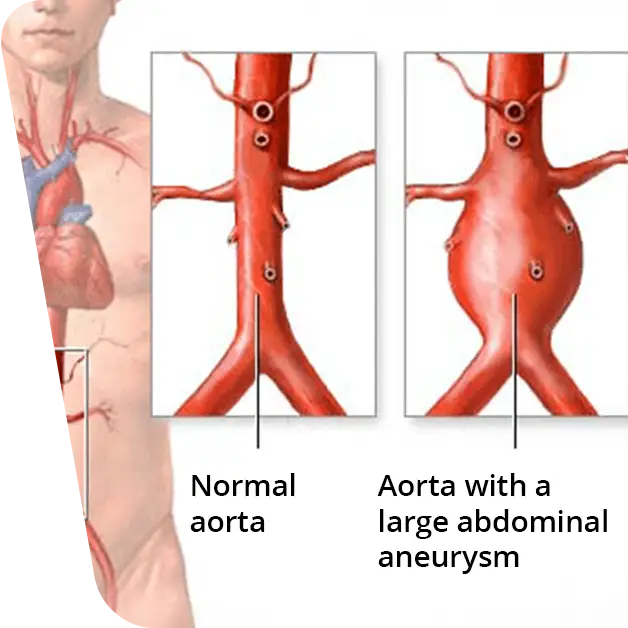
What are the types of hiatal hernias:
- By gliding – represents the return of the gastric junction.
- Paraesophageal – represents the return of a portion of the stomach.
- Mixed – combination of the above two.
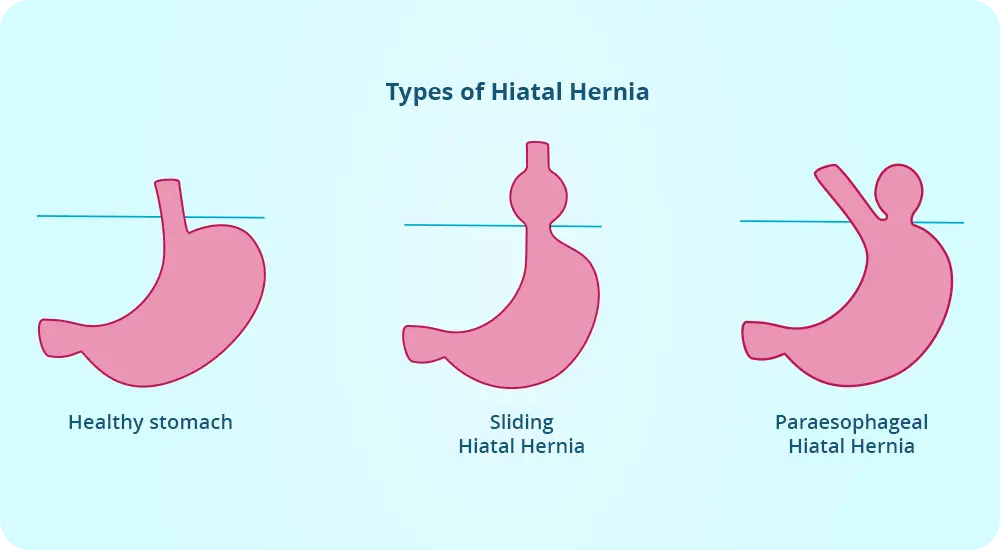
The most common form of hiatal hernia is a sliding hernia. The paraoesophageal form is less common, but can give serious complications such as strangulation or obstruction in the digestive tract.
This anomaly can also be classified according to the size of the hernia (the portion that turns). Small hiatal hernias may be present in a large proportion of patients without them experiencing any problems or symptoms. In contrast, a large hernia can cause discomfort to patients by allowing gastric contents to return to the upper floors of the digestive tract.
Table of contents
ToggleWhat are the symptoms and complications of hiatal hernia?
Most small hernias do not cause any discomfort to the patient. But large hiatal hernias can cause:
- The sensation of gastric burning, called pyrosis, is aggravated by leaning forward or lying on the back.
- Chest or abdominal pain, often after eating.
- Regurgitation of fluids or food.
- Backflow of stomach acid into the esophagus.
- Difficulty swallowing.
- Difficulty breathing.
- Bloody vomit, resembling coffee grounds, or the appearance of black stools, which may indicate gastrointestinal bleeding.
- Feeling of stomach fullness and early satiety during meals.
Complications that hiatal hernia can bring are hemorrhage, where patients may feel tired due to blood loss. This hemorrhage occurs as a result of damage to the digestive tract from the edges of the diaphragmatic opening.
In some cases a para-esophageal hernia may tighten excessively at the site of sliding into the chest cavity and remain there (incarceration). In this situation the gastric wall will receive less blood and still become strangulated. Patients will experience severe chest pain and increased difficulty in swallowing. Of course, at this point immediate medical treatment is necessary.
What causes hiatal hernia?
The exact cause of this abnormality is not entirely known. However, there are certain cases that can lead to its occurrence:
- Trauma or a history of surgery.
- High pressure in the abdomen caused by lifting heavy objects or childbirth and obesity (recommended article: What are the benefits of bariatric surgery).
- The presence of an enlarged diaphragmatic ring at birth.
In addition to these causes, risk factors may also be present: smoking, old age.
How is a hiatal hernia diagnosed?
First, your doctor will ask you if you have experienced the symptoms described above. Next, some paraclinical diagnostic modalities may be included such as:
- Upper digestive endoscopy – your doctor will insert a thin tube into your mouth with a camera at the top, which will transmit real-time images of your esophagus and stomach; any changes in the structure of your digestive tract will be visible.
- Barium X-ray – you will be asked to drink a solution containing barium, and then an X-ray will be taken, giving images that will allow the doctor to see the position of the digestive tract.
What are the treatment options for hiatal hernia?
Hiatal hernia treatment: Depending on the severity of the symptoms, a prescription for medication or surgery will be recommended.
Drug treatment
Will try to relieve symptoms such as pyrosis and acid reflux, using antacid drugs (neutralizes stomach acidity), drugs that reduce stomach acid production, drugs that will block stomach acid production and allow the esophagus to heal.
Surgical treatment
Is necessary if symptoms are severe, medication does not have the desired effect or there is a risk of complications. General surgery is a particularly important section of the VenArt clinic. More details in the general surgery section.
How is the surgery performed?
There are 3 ways to approach hiatal hernia: open, laparoscopic or endoluminal surgery. In all cases general anesthesia is required.
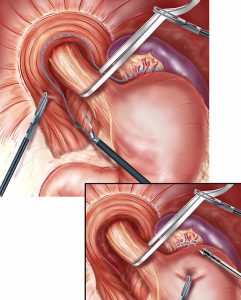
Laparoscopic surgery
This operation is minimally invasive, requiring only a few small incisions in the abdomen. Through these, the surgeon will insert the laparoscope, which is a thin tube fitted with a light source and a camera. This will repair the hernia and possibly strengthen the diaphragmatic opening to prevent the stomach from coming back.
Laparoscopic hiatal hernia surgery has certain advantages over other surgical approaches:
- Lower risk of infection.
- Less painful.
- Less visible scarring.
- Faster recovery.
- Better results.
Open surgery
This is a more invasive approach, as it requires a large incision to be made to repair the hernia. The surgeon’s aim is to position the stomach in place and wrap it around the distal portion of the esophagus to strengthen the walls of the digestive tract at this level, thus preventing stomach acid from returning into the esophagus.
Endoluminal fundoplication
This is a newer approach and is the least invasive of the options. No incisions will be made, instead an endoscope will be inserted into the esophagus. Then the surgeon will attach small clips to the place where the esophagus meets the stomach. These clips will prevent acid and food returning back into the esophagus. It is worth mentioning that this surgery can only be performed on certain patients.
A medical cliché says that the best treatment is prevention, however hiatal hernia is hard to prevent. So in this case the medical advice is to tell patients to minimize factors that may increase the risk of developing the disease: avoid sedentary lifestyles, do not lie down immediately after eating, do not do sports activities immediately after eating, but wait 2-3 hours.
Dr. Oleg Cebotari
Doctor of Medical Sciences with a PhD thesis entitled “Intestinal resections in non-specific inflammatory bowel diseases”, Dr. Cebotari benefits from an extensive postgraduate training, attending specialization courses both in the country and abroad, Germany Heidelberg.
With a young and innovative spirit, he performs with exceptional results surgical procedures both in the field of classical and laparoscopic surgery, being considered a reference name in his specialty.
Symptoms of Hiatal Hernia
Most patients with hiatal hernia through slippage are asymptomatic, but sometimes chest pain and other symptoms of GER (gastro-esophageal reflux disease) can occur. Paraoesophageal hiatal hernia is generally asymptomatic, but unlike sliding hiatal hernia, it can incarcerate and strangulate. Both types of hiatal hernias can result in massive or occult digestive hemorrhage.
Diagnosis of Hiatal Hernia
A large hiatal hernia is usually discovered by accident by chest X-ray examination. A small hiatal hernia is diagnosed by a barium transit.
Hiatal hernia can be classified as follows:
- By sliding (axial, cardio-esophageal) when the upper sphincter, called the cardia, passes together with the thoracic stomach;
- By rolling (paraoesophageal) – when the bottom of the stomach passes into the thorax past the esophagus, without the cardia;
- Mixed.
Complications of paraoesophageal hernia
The most common are digestive microhemorrhages with the occurrence of secondary anemia, which is identified in 55% of cases. On the herniated stomach pouch, ulcers may occur, which in turn may be complicated by bleeding or perforation.
Gastric volvulus (twisting of the stomach around its axis) is a major complication that is manifested by 3 signs:
- Intense pain;
- Ineffective vomiting effort;
- Impossibility of placing the gastric tube.
On the barite transit, 2 overlapping, fluid-level pouches are distinctly visible. If strangulation occurs on the volvulus, the patient may also present thoracic signs (difficult breathing with abnormal noises at the base of the lungs). The most fatal complication is necrosis associated with perforation (50% mortality).