Post-Thrombotic Syndrome (PTS) is a challenging complication following deep vein thrombosis (DVT), particularly affecting the pelvic veins. Patients often experience debilitating symptoms like chronic pain, swelling, and even venous ulcers. However, the advent of venous stenting has emerged as a promising intervention, offering new hope and improved quality of life for those affected by this condition.
Table of contents
ToggleUnderstanding Post-Thrombotic Syndrome
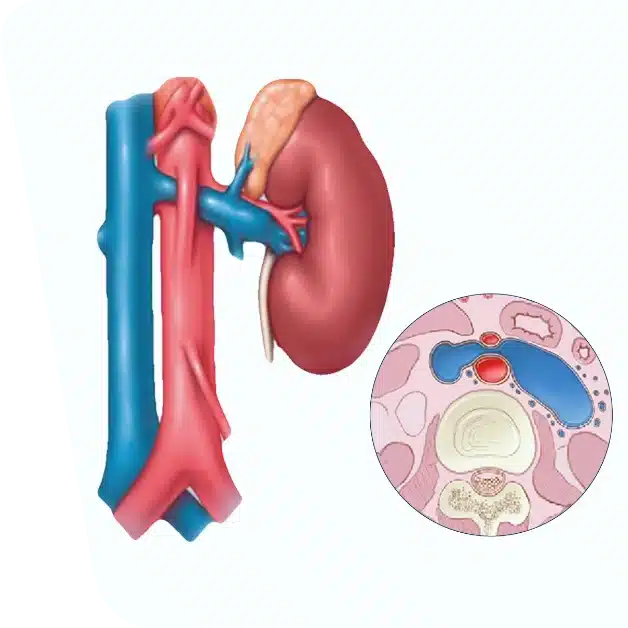
Post-Thrombotic Syndrome is a long-term consequence of DVT, a condition where blood clots form in the deep veins, often in the legs or pelvis. PTS develops in up to 50% of individuals with DVT and significantly impacts daily activities due to chronic pain, swelling, and in severe cases, venous ulcers.
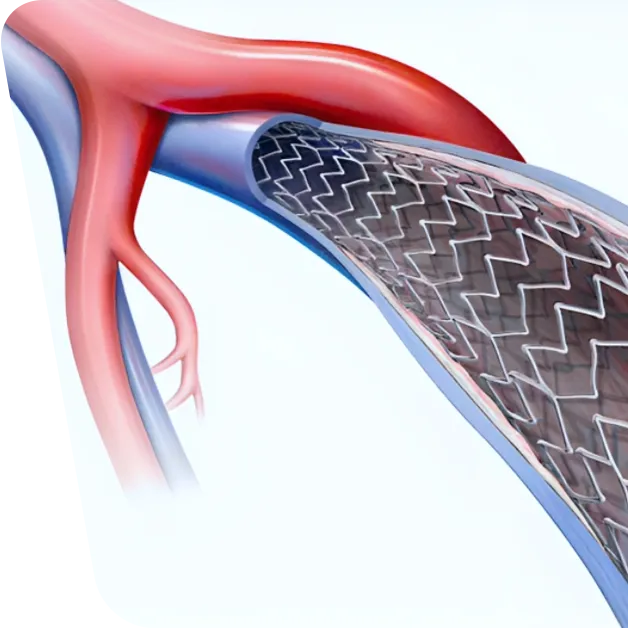
The Role of Venous Stenting in PTS
Venous stenting has become increasingly significant in managing PTS, especially in cases involving pelvic veins. This minimally invasive procedure involves inserting a stent – a small, mesh-like tube – into the affected vein to keep it open and improve blood flow.
Benefits of Venous Stenting for Pelvic Vein
- Alleviating Symptoms: Venous stenting can significantly reduce the symptoms associated with PTS, including pain, swelling, and skin changes.
- Minimally Invasive: Compared to traditional surgical options, venous stenting is less invasive, leading to quicker recovery times and less discomfort.
- Improved Quality of Life: Patients often experience a marked improvement in their quality of life, regaining mobility and comfort.
- Reduced Risk of Recurrence: Stenting can help prevent the recurrence of blood clots in the treated area, offering long-term benefits.
The Procedure: What to Expect
During the venous stenting procedure, a small incision is made, usually in the groin area. Using imaging guidance, a catheter is navigated to the affected vein. The stent is then placed to hold the vein open and restore normal blood flow. The procedure typically takes 1-2 hours and is often performed under local anesthesia.
Ideal Candidates for Venous Stenting
Not every patient with PTS is a candidate for venous stenting. Ideal candidates usually have:
- Chronic symptoms not responding to conservative treatments like compression stockings.
- Evidence of significant vein blockage or narrowing on imaging studies.
- Good overall health to undergo the procedure.
Post-Procedure Care and Follow-Up
After venous stenting, patients may need to wear compression stockings and take blood thinners to prevent new clots. Regular follow-up appointments are crucial to monitor the stent and overall vein health.
Risks and Considerations
As with any medical procedure, venous stenting carries some risks, including bleeding, infection, and blood clots. It’s important to discuss these risks with a healthcare provider.
Conclusion
Venous stenting for pelvic vein PTS represents a significant advancement in treating this debilitating condition. By offering a minimally invasive solution with lasting benefits, this technique has transformed the management of PTS, giving patients a new lease on life.